We are short staffed in our hospital right now. Covid-19, you might say, is causing all the nurses to leave. But is it?
A nurse friend of mine was recently called into her manager’s office. It had been a hard month in the CCU; every day was short staffed with high acuity patients. Every day was staffed by primary nurses only – no CNAs or LPNs to help. She had been communicating the unsafe staffing ratio with her manager and found the manager unresponsive to the messages. My friend has been working for that hospital for over 7 years and wasn’t really looking to leave the position. She felt that her work family was dear to her (with the exception of a few bad eggs) but for the most part, she adored everyone there. Here is how this scenario played out:
Manager: I’ve had a lot of complaints about you.
Nurse Friend: Me? Really? (she relayed that she was floored by this)
Manager: Yes, it was overheard that you refuse to get credentialed in bedside sedation procedures.
Nurse Friend: Yes, right now I do. That’s no secret. If I get credentialed in this, I will be required to do ALL the procedures which are one-on-one patients, and that is unsafe as I will also have my other three critical patients….
Manager (dismisses this) You also go around all day long telling people that you want to go home. Is there something wrong with you I need to know about?
Nurse Friend, again, stumped. “I don’t say I want to go home any more than anyone else?…? I guess I am worried about money and my life?
Manager: Well, several people have complained.
Nurse Friend: Well, it has been really awful up here lately. No one has not complained. There isn’t enough time in the day to do everything that we need to do and the ratios are unsafe…
Manager: You don’t hear of my ED nurses complaining when they have 4 patients to take care of.
Nurse Friend (had nothing to say about that, as she had received half dead, soiled dirty patients with 24g IVs from the ED many times. She also knew that most of the ED nurses left to go to float pool. The ED was the main culprit over why they never had a CNA in the CCU as well, as the ED frequently pulled their ancillary staff down there. No words)
The result of this meeting, which was in the middle of my friend’s 10 minute lunch attempt, was that she was demoted from her charge nurse position. She had never once gotten a write up in that company. She never once was approached by ANY of the “complainers” about the scenarios that were complained about. There was never an official complaint, never a performance review, never any sort of disclipinary action of ANY KIND. But apparently, without her knowledge, there was an upper management meeting about my nurse friend and she was accused, judged, and sentenced without a representative or a trial. All on complaints from “other people”.
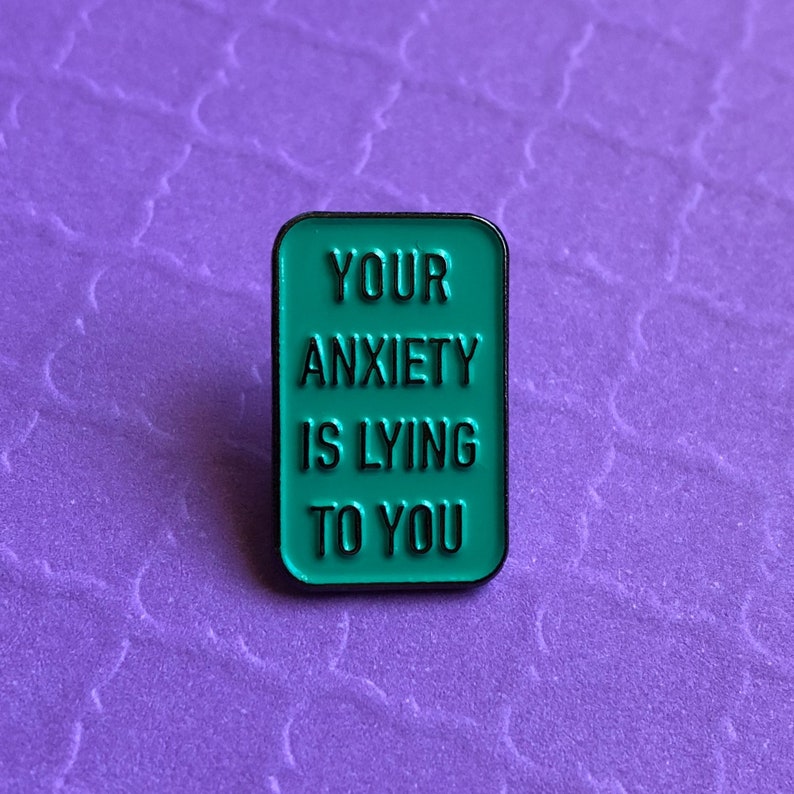
She left that meeting emotionally devastated and is now unable to trust anyone in her work home. Everyone that was before a friend is now a person of suspicion, and her happy nature that was full of love for her work family has been shot down and killed. She is unhappy, crushed, and confesses that she can never trust anyone at that place of employment ever again. One of her biggest upsets is the CNO, who she knew to be a born-again Christian, no longer responds or comments to any of her emails or Facebook posts. She is confused and deeply hurt at the actions and back-stabbing that was taken as gospel truth. No one ever spoke with her on a personal level. How unprofessional.
But is this scenario uncommon? Personal sources that have since come to me since this incident proves that this happens all too often in the medical field. This sort of gossip and hearsay has damaged several people and their careers. When I told this story to some of my peers, many people related to it with first-hand accounts of their own similar stories of hurtful co-workers and management that turned against the worker.
Perhaps THIS is why nurses are leaving? The going gets tough, but management doesn’t do a thing to help. Or find out what is going on. They set the SAME STANDARDS as pre-pandemic times and expect their nurses to comply and perform at the same level. It is not fair. It is not safe. It is not professional.
Managers and Administrators. STEP UP. Stop putting up “Heroes Work Here” signs and step onto your units and find out FIRST HAND what is going on with your employees. YOU are the reason people are leaving. NOT sicker patients.